Abstract
Background: In a developing country with limited resources and insurance coverage, it is very important to risk stratify patients early in the treatment of Acute Lymphoblastic Leukemia (ALL). This strategy will enable better utilization of resources and also identify a subset of patients who will benefit from early haematopoeitic stem cell transplant (HSCT). Historically, clinical and laboratory features such as age, gender, white blood cell counts at diagnosis, organomegaly, mediastinal mass, morphology, immunophenotyping and cytogenetics have been used to assess the outcome of patients with ALL. However recent studies have shown that assessment of minimal residual disease (MRD) was the most important prognostic determinants of both childhood and adult ALL. Currently multiparameter flow cytometry and quantitative polymerase chain reaction (PCR) of the immunoglobulin or TCR genes are most commonly used for the assessment of MRD. However availability of this technology is very limited. In this present study, we assessed the MRD at day 33 post induction chemotherapy by flowcytometry at our center, and risk stratified patients to determine outcomes.
Methods: We analyzed a cohort of 70 de novo ALL patients who presented to our Hospital (Mazumdar Shaw Medical Center, Narayana Health City, Bangalore, India) between April 2014 and April 2017. Diagnosis was confirmed by bone marrow aspiration based on the morphology, cytochemistry, immunophenotyping and cytogenetics. Clinico-pathological features, immunophenotyping, cytogenetics were recorded at the time of presentation. Day 8 prednisolone response was recorded and MRD assessment was done at day 33, using 8 Color multiparameter Flowcytometry. The cost of MRD analysis is 220 US$.
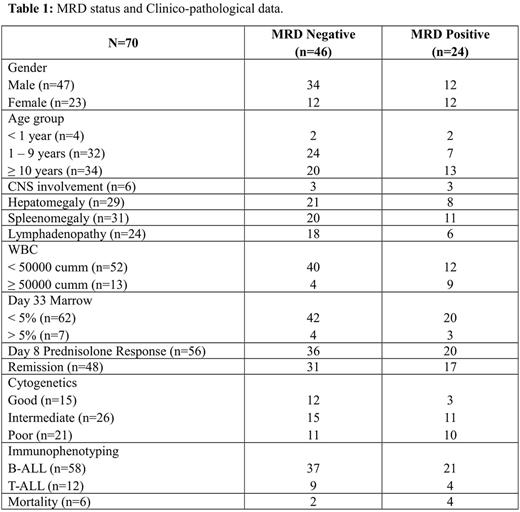
Results: Out of 70 patients, 47 (67%) were male. The median age was 9 years (range: 8 months, 69 years). Among the subtypes, B-ALL was found in 83% (n=58) and T-ALL in 17% (n=12). The most common presenting symptom was fever (66%). Hepatosplenomegaly was seen in 35% (n=23), lymphadenopathy in 35% (n=24). CNS involvement at presentation was seen in 8.6% (n=6). The median WBC count at presentation was 11x103/µl (0.8-437). Majority of adults (39%) and pediatric patients (44%) had normal cytogenetics. This was followed by hyperdiploidy (27%, n=11) in children and t(9;22) in adults (26%, n=6). Intermediate risk cytogenetics were seen in most of the patients (44%, n=26). 57 patients (81%) showed good prednisolone response at day 8. Twenty-seven (40%) patients were MRD positive at day 33. Among the MRD positive cases, nearly 50% patients were aged <1 yr or >10 yr. Seventy-five percent of patients in the age group between 1-9 yrs were MRD negative. 72% patients with WBC >50x103/µl, 40% of patients with CNS involvement and 50% of patients with PPR group had MRD positivity. The incidence of MRD positivity was similar in both B-ALL and T-ALL patients (40% vs 42%). The MRD status and clinical details are summarized in table 1. The disease free survival was significantly higher in MRD negative patients compared to MRD positive patients at 24 months (97% vs 58%, p<0.01) (Figure 1).
CONCLUSION: MRD assessment at day 33 post chemotherapy is the most important factor in determining risk of relapse in patients with ALL, surpassing the prognostic information obtained from analysis of pretreatment characteristics alone. This determinant helps to take the decision on offering stem cell transplant to MRD positive patients, on the background of resource constraints, and poor outcomes of CR2 transplants.
Figure 1: Overall Survival at 24 months: MRD positive vs. MRD negative
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal